“
If you live long enough, it's like death and taxes - you will likely get
OSTEOARTHRITIS
Dr. Todd Stitik
Overview
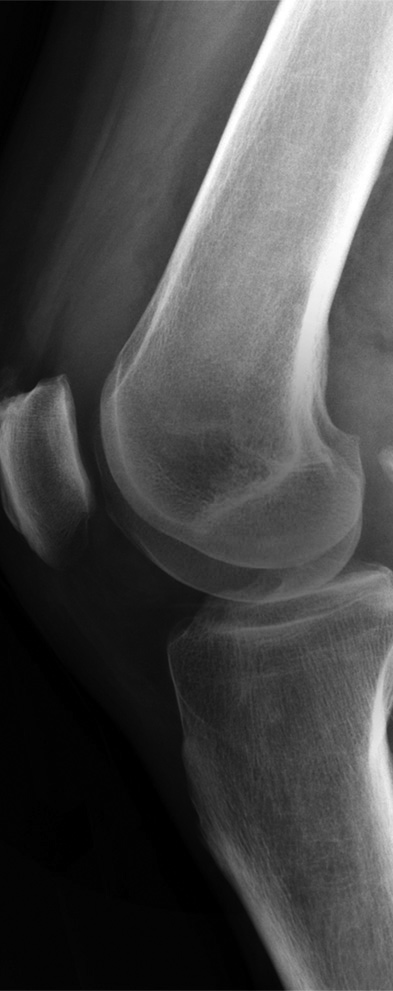
Sometimes called degenerative joint disease or degenerative arthritis, osteoarthritis (OA) is the most common chronic condition of the joints, affecting millions of Patients Worldwide. Although osteoarthritis can damage any joint in your body, the disorder most commonly affects joints in your hands, knees, hips and spine. The overall incidence of osteoarthritis is similar for males and females, and is strongly associated with age. Osteoarthritis occurs in two general forms, "primary" in which the underlying cause is not known, and "secondary" where a precipitating cause, such as trauma, can be identified. The majority of cases are classified as primary. All articular tissues have dysregulation of local turnover and repair processes and consequent joint failure. Pathologic aspects are represented by focal degeneration and progressive loss of cartilage and hypertrophy of the subchondral bone, joint margin, and capsule.
Osteoarthritis symptoms can usually be effectively managed, although the underlying process cannot be reversed. Staying active, maintaining a healthy weight and other treatments may slow progression of the disease and help improve pain and joint function.
Who’s Affected?
Although OA occurs in people of all ages, osteoarthritis is most common in people older than 65. Common risk factors include increasing age, obesity, previous joint injury, overuse of the joint, weak thigh muscles, and genes.
- One in two adults will develop symptoms of knee OA during their lives.
- One in four adults will development symp toms of hip OA by age 85.
- One in 12 people 60 years or older have hand OA.
Risk factors
Factors that may increase your risk of osteoarthritis include:
- Older age. The risk of osteoarthritis in creases with age.
- Sex. Women are more likely to develop osteoarthritis, though it isn't clear why.
- Obesity. Carrying extra body weight con tributes to osteoarthritis in several ways.
- Joint injuries. Injuries, such as those that occur when playing sports or from an accident, may increase the risk of OA
- Certain occupations. If your job includes tasks that place repetitive stress on a par ticular joint, that joint may eventually de velop osteoarthritis.
- Bone deformities. Some people are born with malformed joints or defective carti lage, which can increase the risk of OA.